Strategies & goals in care team communications
A recent survey found that improving communication among the care team is a key step in battling rising rates of clinician burnout and producing positive ripple effects for both workers and patients.
The 2021 survey by healthcare communications firm Spok analyzed clinical communication trends and challenges and found that connecting caregivers with team members and the information they need is crucial to job satisfaction and patient experience. Many respondents also believed clinician burnout could be tackled in part by enhancing communications among care teams. (See Caring for Caregivers for more on the effects of burnout on caregivers.)

Reaching these goals requires that healthcare organizations steadfastly focus on improving communications efforts and workflow, says Annabaker Garber, Ph.D., RN, Chief Nursing Informatics Officer and VP, HCA Healthcare (retired in April 2022).
“While efficient communications doesn’t do anything directly to get rid of burnout, it can dial down frustration, which is a big contributor to burnout,” Garber explains. “People are leaving the healthcare community because the work is extremely complex, but they also don’t necessarily have the right tools to do their job and can’t always get all the information they need to make decisions.
“It’s death by a thousand paper cuts,” she adds. “Clinical communications tools can help.”
The importance of secure & user-friendly tools
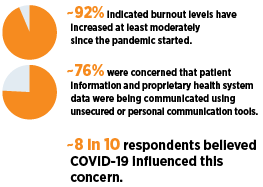 The Spok survey, which compiled input from more than 200 physicians, nurses, executives and other healthcare workers, revealed fundamental attitudes about the state of communication within their respective organizations.
The Spok survey, which compiled input from more than 200 physicians, nurses, executives and other healthcare workers, revealed fundamental attitudes about the state of communication within their respective organizations.
Secure, appropriate communications tools can “cut out a lot of steps that add to people’s sense of frustration,” Garber says. HCA Healthcare took aim at this issue several years ago, leveraging secure smartphone technology for care teams through its “Mobile Heartbeat” program.
The initiative has since been implemented in more than 140 hospitals via 75,000 shared devices.
Increasing workflow efficiency was cited as the top way to combat clinician burnout in the Spok report. Garber says Mobile Heartbeat has achieved this by facilitating and prioritizing key processes. These include admissions as an inpatient from the emergency department, pending patient discharges, intradepartmental communication when assistance is needed, coordination of radiology exams and many other aspects of clinical communications that have led to higher job satisfaction for clinicians and better experiences for patients.
“It gets patients transported faster and expedites the ability to get them to the next stage of care,” she says. “If a doctor can talk with a nurse sooner, they’re more likely to get orders in faster. It also gets stat blood and imaging services done quicker because you’ve expedited the communications. There are many operational benefits in addition to a morale component.”
 Using tools effectively
Using tools effectively
Which tactics can healthcare organizations use to improve communications among care teams and streamline workflow? The first step, Garber says, is identifying “pain points” where the current system doesn’t work.
“The best way to take full advantage of your system is to figure out what work you want to expedite and where slow communications are causing problems,” she says. “There’s nothing like putting your boots on the ground. You have to be thoughtful about talking to people and documenting how they want communication to be better.”
Garber notes that smartphone features that facilitate “global” texting among care teams are often a boon for facilities. “Just like a group chat speeds up the decision about where everyone decides to go for dinner, it does the same thing for workflow,” she explains.
But “alarm fatigue” from alerts that broadcast changes in things from a patient’s condition to a staff alert can sabotage this type of instant communication, so organizations shouldn’t overuse it, Garber notes.
“They blame it on the tool, not on the fact that they’re using the tool poorly,” she says. “They don’t use it to its highest potential because they’re not necessarily willing to govern it.”
Along those lines, healthcare organizations should be intentional about distinguishing between clinical and social communication. For example, sharing information about a patient whose condition has deteriorated should be done during an in-person conversation, not via text.
“There’s an etiquette to it, and you have to set up that etiquette and expect employees to adhere to it,” she adds. “It’s a clinical process and, like any other, has to be led by the clinical leadership of a facility. Expectations of behavior such as politeness and responsivity have to be thought of as a clinical process, not a social process.”
Learn more about caring for caregivers and strategies for reducing burnout.
Share Email Communications, Employee Training, Q2 2022